

Andrew Kau, MD, PhD, studies the interaction between airway microbiota and host factors such as gender or obesity in order to better understand the risk for chronic asthma and other allergic diseases.
Asthma airway microbiota can play a critical role in the development of chronic asthma. Researchers in the Kau Lab are specifically investigating how the gastrointestinal and airway microbiomes increase susceptibility for the development of allergic airway diseases.
Current research in the lab is focused on better understanding how specific microbes alter allergic immune responses. The lab also is involved in a clinical study comparing the gastrointestinal and airway microbiomes of healthy and asthmatic men and women to see if there are gender differences in how microbial ecology may impact mucosal immune function.
The ongoing research has led the development of new computational, microbiologic and sequencing tools to delve into the complex interrelationships between host factors and microbial ecosystems.
The Kau lab is part of the Center for Women’s Infectious Disease Research in the Division of Allergy and Immunology and the Department of Medicine at Washington University School of Medicine.
Lab Team
Andrew L. Kau, MD, PhD
Principal Investigator
Research Technicians
Anne Rosen
Research Technician II
Michael Lint
Research Technician II
Jamison Rucker
Research Technician II
Current Graduate Students
Ariel Hernandez Leyva
MSTP Student
Naomi Wilson
PhD Student
Jesus Santiago Borges
PhD Student
Select Publications
- Cell Rep. 2020 Nov 3;33(5):108331. doi: 10.1016/j.celrep.2020.108331.
- PLoS Pathog. 2019 Apr 25;15(4):e1007645. doi: 10.1371/journal.ppat.1007645.
- Sci Transl Med. 2015 Feb 25;7(276):276ra24. doi: 10.1126/scitranslmed.aaa4877.
Coming soon.

Research in the laboratory of Brian J. Laidlaw, PhD, focuses on understanding how immunological memory develops in order to identify new approaches to protect against newly emerging viruses and allergic disease.
Specifically, researchers in the lab study the transcriptional pathways that regulate the development and function of memory B cells. While memory B cells are essential for the induction of protective immunity following vaccination, unrestrained development of memory B cells can result in the induction of pathological states, such as allergic disease. Laidlaw is a pioneer in the field, having been the first to characterize memory B cell precursor cells while a postdoctoral fellow at the University of California-San Francisco. He subsequently developed the first in vivo method to screen factors driving memory B cell development and identified several transcription factors that modulate the development of memory B cells following viral infection.
Current Research
The Laidlaw lab uses advanced cellular immunology and sequencing approaches to identify novel regulators of memory B cell development and function.
One area of focus is understanding how the memory B cell response to viral infection and allergic disease is shaped by the tissue microenvironment. For example, the lab investigates the process by which memory B cells develop in the lungs following influenza infection. Lung-resident memory B cells are important regulators of protective immunity against influenza virus but are not induced by current vaccination approaches. Identification of how lung-resident memory B cells develop would enable new vaccination approaches that could promote enhanced protective immunity.
The lab uses Crispr-Cas9 and other genetic approaches to identify transcription factors driving memory B cell development and function. Understanding of the mechanisms by which these factors function will reveal new targets for therapies designed to enhance the B cell response and protect against newly emerging viral strains. Identification of novel therapeutic targets will also facilitate new approaches to resolve allergic disease by restricting memory B cell development and limiting the induction of pathogenic IgE antibodies.
Research in the lab is currently funded by an NIH/NIAID K22 career research grant.
Laboratory Team
Brian J. Laidlaw, PhD
Principal Investigator
Brittany Henry
Research Tech II
Chris Hanson
Research Tech II
Serena Chan
Undergraduate researcher
Frank Lin
Undergraduate researcher
Haley Pak
Undergraduate researcher
Select Publications
- Laidlaw, B.J.*, and Cyster, J. (2020). Transcriptional regulation of memory B cell differentiation. Nat. Rev.Immunol. 1-12. *Corresponding Author
- Laidlaw, B.J., Duan. L., Xu, Y., Vazquez, S.E., and Cyster, J. (2020) The transcription factor Hhex cooperates with the corepressor Tle3 to promote memory B cell development. Nat. Immunol. 21, 1082-1093. PMCID: PMC7442689
- Laidlaw, B.J., Schmidt, T.H., Green, J.A., Allen, C.D.C., Okada, T., and Cyster, J. (2017) The Eph-related tyrosine kinase ligand Ephrin-B1 marks germinal center and memory precursor B cells. J. Exp. Med. 214 (3), 639–649. PMCID: PMC5339677
- Laidlaw, B.J., Gray, E.E., Zhang, Y., Ramirez-Valle, F., and Cyster, J. (2019) Sphingosine-1 phosphate receptor 2 restrains egress of gd T cells from the skin. J. Exp. Med. 216 (7), 1487-1496. PMCID: PMC6605748
- Laidlaw, B.J., Lu. Y., Amezquita, R.A., Weinstein, J.S., Vander Heiden J.A., Gupta, N.T., Kaech, S.M., and Craft, J. (2017). Interleukin-10 from CD4+ follicular regulatory T cells promotes the germinal center response. Sci. Immunol. 2 (16), eaan4767. PMCID: PMC5846620

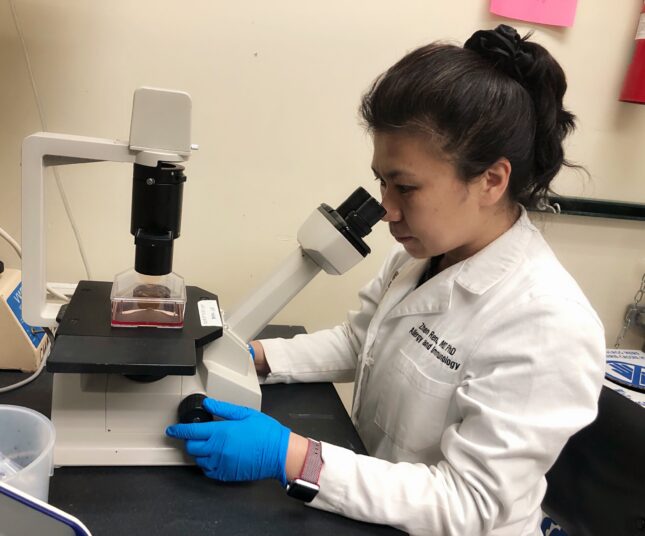
Zhen Ren, MD, PhD, studies hereditary angioedema (HAE) and angioedema of unknown cause (AUC). She searches for biomarkers to better diagnose and treat AUC while also investigating the genomic associations that lead to clinical variability in patients with HAE.
HAE is a rare genetic disorder that presents as recurrent, unpredictable episodes of tissue swelling. More than half of all patients diagnosed with HAE experience laryngeal attacks, which can be life-threatening due to asphyxiation. There is, however, substantial variability in symptoms experienced among HAE patients. Some have frequent attacks while others have few.
Ren’s research focuses on the genetic and molecular mechanisms underlying the clinical variability among HAE patients. The pathogenesis of HAE is linked to mutations in the C1 esterase inhibitor (C1INH). A decrease in C1INH leads to over-production of bradykinin (BK), which causes increased vascular permeability and swelling. However, the level of C1INH does not predict which patients are more likely to experience severe angioedema attacks. In addition, an increasing number of HAE cases have normal functional C1INH. There are no available molecular diagnostic markers that can be used to diagnose these individuals, resulting in cases falling into the category of Angioedema of Unknown Cause (AUC). Ren’s research will potentially identify new biomarkers that can be used to diagnose patients with AUC.
Clinically, the Division of Allergy and Immunology oversees one of the largest centers in the Midwest dedicated to treatment and research of hereditary angioedema. Within the center, multiple pharmaceutical trials have led to FDA-approval of several prophylactic medications to treat the disease. There are numerous clinical trials under way in our clinical research center, including prophylactic therapy for non-histaminergic angioedema with normal C1-INH level, oral long-term prophylactic treatment for HAE and oral treatment for acute attacks of HAE.
Principal Investigator
Zhen Ren, MD, PhD
Instructor in Medicine
Division of Allergy and Immunology
Washington University School of Medicine

Aaron Ver Heul, MD, PhD, investigates the neuroimmune basis of allergic inflammation, with a special emphasis on conditions that have itch as a primary symptom, including chronic hives (chronic spontaneous urticaria). The goal is to enhance understanding of the underlying mechanisms that shape both immune and neurological responses to itch.
Chronic spontaneous urticaria (CSU) is an allergic itch condition characterized by recurrent bouts of itchy hives (wheals) and/or swelling (angioedema) and exaggerated mast cell responses that can last weeks, if not years. Antihistamines are the typical treatment options; however more than half of all patients do not see relief from their symptoms with antihistamines alone.
Ver Heul runs a translational specialty clinic for treatment of urticaria. He is particularly interested in understanding why some patients with CSU have symptoms that are more difficult to control so that better treatments can be developed. As part of this effort, he currently oversees a pharmaceutical clinical trial to test the effectiveness of a new monoclonal antibody medication in patients with CSU. A key part of this trial is aimed at finding out if this new medication can improve CSU in patients who have failed other therapies. Patients interested in contributing to Ver Heul’s translational or clinical research on CSU are welcome to schedule an appointment for further evaluation.
Complementing the clinical research is a laboratory research effort focused on mast cell biology. Mast cells are highly responsive to interleukin-33 (IL-33), which is increased in a variety of inflammatory skin diseases, including chronic hives. Ver Heul has developed new mouse models of itch and allergic inflammation and now is evaluating whether IL-33 broadly amplifies itch responses in mouse models. His background in biochemistry, structural biology, neuroimmunology, mucosal immunology, and allergy and immunology is ideal to study itch biology and the emerging field of functional neuroimmunology.
Ver Heul recently started his own research group after finishing post-doctoral training in the research lab of Brian Kim, MD, MTR, FAAD, Sol and Clara Kest Professor of dermatology and director of the Mark Lebwohl Center for Neuroinflammation and Sensation at the Icahn School of Medicine at Mount Sinai. The Kim Lab was the first to characterize two distinct pathways by which mast cells can be activated to cause itch. Taking that research further, Ver Heul hopes to develop new models of urticaria that lead to a greater understanding of both mast cell biology and the inter-connectedness between allergic inflammation and the nervous system to identify new therapeutic targets that could lead to more effective clinical treatments.
Principal Investigator
Select Publications
- Jain, U., Ver Heul, A., Xiong, S., Martin, G.H., Demers, E.G., Kern, J.T., Lai, C.-W., Muegge, B.D., Barisas, D.A.G, Leal-Ekman, J.S., Parakkal, D., Ciorba, M.A., Liu, T.-C., Hogan, D.A, Debbas, P., Braun, J., McGovern, D.P.B, Underhill, D.M., and Stappenbeck, T.S. Debaryomyces is enriched in Crohn’s disease intestinal tissue and impairs healing in mice. Science (2021) [accepted].
- Wang, F., Trier, A.M., Li, F., Kim, S., Chen, Z., Chai, J.N., Mack, M.R., Morrison, S.A., Hamilton, J.R., Baek, J., Yang, T.-L.B., Ver Heul, A., Xie, Z., Dong, X., Kubo, M., Hu, H., Hsieh, C.-S., Dong, X., Liu, Q., Margolis, D.J., Ardeleanu, M., Miller, M.J., Kim, B.S. A Basophil-Neuronal Axis Promotes Itch. Cell 184, 422-440.e17 (2021).
- Tamari, M., Ver Heul, A., Kim, B.S. Immunosensation: Neuroimmune Cross Talk in the Skin Annu Rev Immunol 39 (2021) [accepted] *co-first authors
- Erickson, S., Ver Heul, A., & Kim, B.S. New and emerging treatments for inflammatory itch. Ann Allergy Asthma Immunol 126, 13–20 (2020).

H. James Wedner, MD, FACP, FAAAAI, is clinically focused on the investigation of rare or orphan immunological diseases such as hereditary angioedema and adult primary and acquired immunodeficiencies. His research center also evaluates new drugs for the treatment of severe asthma.
Wedner’s clinical research is based within The Allergy and Asthma Center (TAAC) at Barnes-Jewish West County Hospital. It is among the largest centers in the Midwest dedicated to advancing therapeutics for hereditary angioedema. The clinical center also follows a large population of primary and secondary immunodeficiency patients. Wedner was the first in Missouri to offer IVIG for the treatment of adult primary immunodeficiencies. Clinical trials currently underway focus on promising treatment options, including oral medications, subcutaneous products, and advanced intravenous immune globulin (IVIG) therapies. A second clinical research center also is located in south St. Louis County and concentrates on clinical trials for severe asthma and other allergic related diseases.
Current Research
Hereditary Angioedema
Hereditary angioedema (HAE) is an extremely rare condition that causes severe swelling in the skin and mucous membranes. These swellings can involve the abdomen, the extremities, and the face and upper airway including the larynx. Left untreated, approximately 45 percent of patients diagnosed with HAE will die of their disease. The disease also increases the risk for the development of autoimmune diseases, most notably lupus erythematosus.
In a majority of cases, HAE is triggered by mutations in the C1NH gene, particularly in Types 1 and 2. In some patients, the symptoms are identical, but there is no abnormality in the C1-inh gene. These are referred to as HAE nl-C1-inh. Over the past decade, multiple pharmaceutical trials conducted within the center and elsewhere have led to FDA-approval of several prophylactic drugs for HAE. These include both injectable and newer oral therapies and new formulations to treat severe episodes (on demand) along with other potential strategies to prevent HAE.
Allergies
A secondary research effort involves investigations into aero-biology, notably pollen, mold, and fungal spores and their allergencity to humans. Dr Wedner and former long-time collaborator Walter Lewis, PhD, a renowned Washington University ethnobotanist and global expert on airborne and allergic pollens, initially began an evaluation decades ago of a weed called Parthenium hysterophorus. The weed,which is commonly found along the U.S. gulf coast, has now been inadvertently transmitted to many other parts of the world. In their first study, Wedner and Lewis determined that Parthenium hysterophorus was an allergenic plant and has cross-reactivity with ragweed. They went on to perform a study of sera from multiple patients provided by allergists along the gulf coast and demonstrated that Parthenium hysterophorus was a major allergen that had been overlooked for many years.
Wedner and Anu Dixit, a post-doctoral fellow in Wedner’s lab, were part of a fungal spore research study funded by the State of Missouri and the Federal Emergency Management Agency (FEMA) after the 1993 flood in the St. Louis region. This study demonstrated the extensive fungal contamination in homes that were flooded throughout the region. It also led to studies of methods for remediation.
Wedner, Lewis and Dixit then became interested in fungal spores in the air around St. Louis and the gulf coast areas. They conducted a large survey of pollen and mold spores in Corpus Christi, Texas over a two-year period from 1996-1998. Data from this survey was then correlated with skin testing from patients who presented to a large allergy practice in the area. The study demonstrated that pollen and mold sensitization differed in the time to sensitization. It also found that fungal contamination was more prevalent than pollen spores in the region and was a leading cause of allergies and asthma.
Cats
Over 20 years ago, Wedner and colleagues began a study of the potential roles of retinoic acid derivatives in decreasing or preventing the secretion of a major cat allergen, Fel D1, as a means of making cats less allergenic. The use of the retinoic acid was of no benefit, but surprisingly, the washing of cats which was used to evaluate the amount of Fel d1 produced by the animals resulted in a significant diminution of Fel D1 levels. Cats, however, do not like to be washed and the method was not widely adopted despite publication of the results. More recently, Wedner and his research group partnered with Nestle-Purina to study the ability of a polyclonal chicken IgY directed against Fel D1 added to cat food to decrease the allergenicity of cats. An environmental chamber study demonstrated the efficacy of the cat food (Wedner, HJ, et al., Feeding cats egg product with polyclonal-anti-Fel d1 antibodies decreases environmental Fel d1 and allergic response: A proof of concept study, J. Allergy and Infectious Diseases, 2021) and a “real life” in-home study has just been completed. These studies led to the marketing of the cat food by Purina.
Principal Investigator
H. James Wedner, MD, FACP, FAAAAI
Dr. Phillip and Arleen Korenblat Professor of Allergy and Immunology in Medicine
Washington University School of Medicine &
Medical Director, The Asthma and Allergy Center, Barnes-Jewish West County Hospital
Select Publications (recent)
- Singh U; Lumry WR; Busse P; Wedner HJ; Banerji A; Craig TJ; Li HH; Tachdjian R; Jacobs JS; Riedl MA; Davis-Lorton M; Christiansen SC; Zuraw BL; Bernstein JA., Association Between Self-Reported Dental Hygiene Practices and Dental Procedure-Related Recurrent Angioedema Attacks in HAE Subjects: A Multi-Center Survey. The Journal of Allergy & Clinical Immunology in Practice. 2020 Jun 10.
- Sleasman JW; Lumry WR; Hussain I; Wedner HJ; Harris JB; Courtney KL; Mondou E; Lin J; Stein MR., Immune globulin subcutaneous, human – klhw 20% for primary humoral immunodeficiency: an open-label, Phase III study., Immunotherapy. 11(16):1371-1386, 2019 11.
- Poole JA; Barnes CS; Demain JG; Bernstein JA; Padukudru MA; Sheehan WJ; Fogelbach GG; Wedner J; Codina R; Levetin E; Cohn JR; Kagen S; Portnoy JM; Nel AE., Impact of weather and climate change with indoor and outdoor air quality in asthma: A Work Group Report of the AAAAI Environmental Exposure and Respiratory Health Committee. [Review], Journal of Allergy & Clinical Immunology. 143(5):1702-1710, 2019 05.
- Satyaraj E, Wedner HJ, Bousquet J., “Keep the cat, change the care pathway: A transformational approach to managing Fel d 1, the major cat allergen.” Allergy. 2019 Oct;74.
Ofer Zimmerman, MD, is interested in genetic susceptibility to infectious diseases, host-pathogen interaction and primary immunodeficiency disorders. Through his research, Zimmerman hopes to identify why particular infections pose a greater risk for some patients but not others.
He is particularly interested in the host-pathogen interaction and evolution of alphaviruses, which are mosquito-transmitted viruses that are responsible for a number of human and animal diseases.
Zimmerman studies Mxra8, a receptor for Chikungunya and other alphaviruses, and the role of human MXRA8 genetic polymorphisms in susceptibility to Chikungunya infection. In addition, Zimmerman researches the connection between Mxra8 structure and function to further define the evolution of alphaviruses.
Zimmerman also studies immune responses to COVID-19 vaccines in patients with primarily immunodeficiency syndromes.
In collaboration with the Division of Infectious Diseases, in a bench to bedside approach, Zimmerman studies genetic susceptibility to mycobacterial and fungal infections.
Principal Investigator
Ofer Zimmerman, MD
Instructor
Division of Allergy and Immunology
Department of Medicine
Washington University School of Medicine
Select Publications
- Kim AS*, Zimmerman O*, Fox JM, Nelson CA, Basore K, Zhang R, Durnell L, Desai C, Bullock C, Deem SL, Oppenheimer J, Shapiro B, Wang T, Cherry S, Coyne CB, Handley SA, Landis MJ, Fremont DH and Diamond MS. An evolutionary insertion in the Mxra8 receptor binding site confers resistance to alphavirus infection and pathogenesis. Cell Host Microbe. 2020 Mar 11;27(3):428-440.e9. doi: 10.1016/j.chom.2020.01.008. Epub 2020 Feb 18. PMID: 32075743
- Zimmerman O, Olbrich P, Uzel G, Freeman AF, Zerbe CS, Rosen LB, Rosenzweig S, Kuehn H, Holmes K, Stephany D, Ding L, Sampaio EP, Hsu AP, Holland SM. STAT1 gain-of-function mutations: high total STAT1 with normal dephosphorylation. Frontiers in Immunology. 2019 Jul.
- Zimmerman O*, Rösler B*, Zerbe CS, Rosen LB, Hsu AP, Uzel G, Freeman AF, Sampaio EP, Rosenzweig SD, Kuhen H, Kim T, Brooks KM, Kumar P, Wang X, Netea MG, Van de Veerdonk FL, Holland SM. Risks of Ruxolitinib in STAT1 gain of function associated severe fungal disease. Open Forum Infect Dis. 2017 Sep 22;4(4): ofx202. doi: 10.1093/ofid/ofx202. eCollection 2017 Fall.